As accessibility remains a top priority for pharmaceutical manufacturers, detailed planning for patient affordability programs is crucial. Join us as we explore actionable insights and practical approaches to optimize the planning process and drive better outcomes for manufacturers, providers, and patients.
Making innovative and life-changing medicines not only accessible but also affordable to patients is pivotal to their wellbeing. As health insurance providers across the world endeavor to control their healthcare spend, access restrictions and patient cost-sharing are expected to become more prevalent.
The result? Patients often face the burden of paying for a portion or even the entirety of direct medication costs. Pharmaceutical manufacturers often seek to bridge this gap by offering patient affordability solutions.
Although there are several forms of patient support, in this article we focus on programs that provide patients financial support to help defray therapy costs. These programs are widespread – our research has identified affordability programs currently offered across global markets by over 20 pharmaceutical manufacturers.
However, the success of these programs varies widely, with significant pitfalls associated with sub-optimal program designs. Pitfalls range from being unable to gain expected pull-through within target patient populations, offering financial assistance that is misaligned with patients’ willingness/ability to pay, and even creation of programs that are not financially viable in the long-term, limiting durability of the patient assistance offered.
Simon-Kucher’s patient affordability planning framework
At Simon-Kucher, we understand that each market presents unique challenges, including variations in healthcare systems, regulatory environments, and socioeconomic dynamics. Our patient affordability planning framework considers key factors that will aid in optimal program design, particularly for ex-US markets.
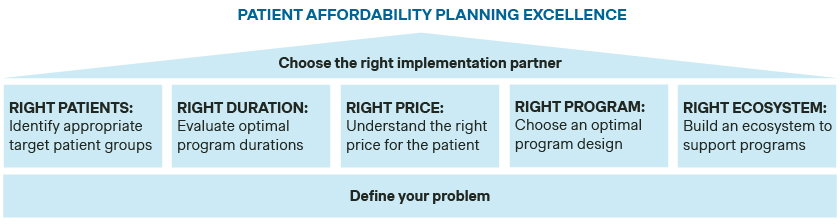
Define your problem
Why does the product in question require a patient affordability program?
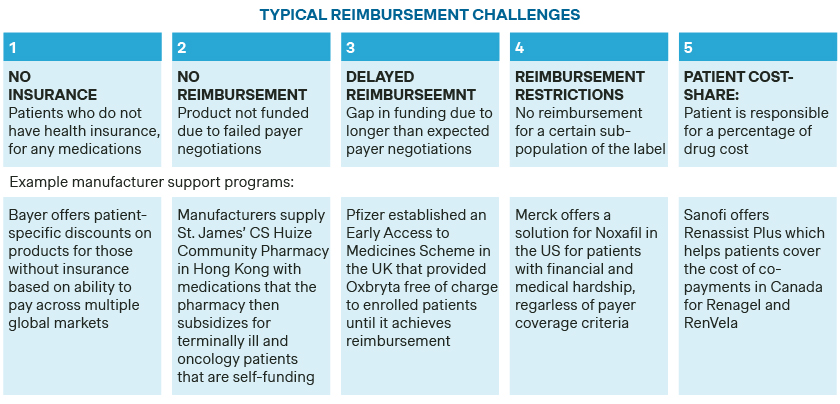
In most markets, there are a range of reimbursement channels available to patients. However, a product can face reimbursement challenges in any of these channels (e.g., with public or private insurance). Characterizing the reimbursement challenges across channels is an important first step.
There are five typical reimbursement challenges:
- Patients not being insured
- No reimbursement for the specific product at all
- Delayed reimbursement
- Reimbursement restrictions
- Patient cost-sharing
Manufacturers should evaluate potential for offering support in all these instances, depending on the product needs. In some cases, for example, if the product is a specialized therapy such as a gene or cell therapy facing full reimbursement hurdles, manufacturers may need to look instead to disease-specific charitable institutions for financial and advocacy support to ensure patient access.
How do current patient dynamics impact product access?
Poor funding is not the only limitation to patient access to medications. Patient attrition often occurs in various parts of the patient journey, such as during symptom awareness, willingness to seek treatment from a physician, and physical access to prescribed medications.
Pharmaceutical companies must have a robust understanding of the patient journey to identify these hurdles. This helps to determine whether additional supportive solutions further upstream in the patient journey are required, ensuring affordability programs have their intended impact.
Do unique market dynamics impact your ability to offer patient affordability programs?
Not all market conditions support patient affordability programs from a regulation or infrastructural standpoint. Legal, reputational, ethical, cultural, supply, and infrastructure dynamics can influence affordability program feasibility and success should be closely evaluated for each market.
In particular, historic reimbursement trends also play a critical role. It is unusual for countries that typically provide universal healthcare coverage, such as western Europe or certain Asian-Pacific countries, to require patient affordability programs. For this reason, patients in such markets can be particularly reluctant to pay out-of-pocket for prescription drugs and there may be a lack of strong precedence for patient affordability programs in such markets. Such challenges need to be accounted for when planning and prioritizing a global patient affordability program roll-out.
Identify the right patients
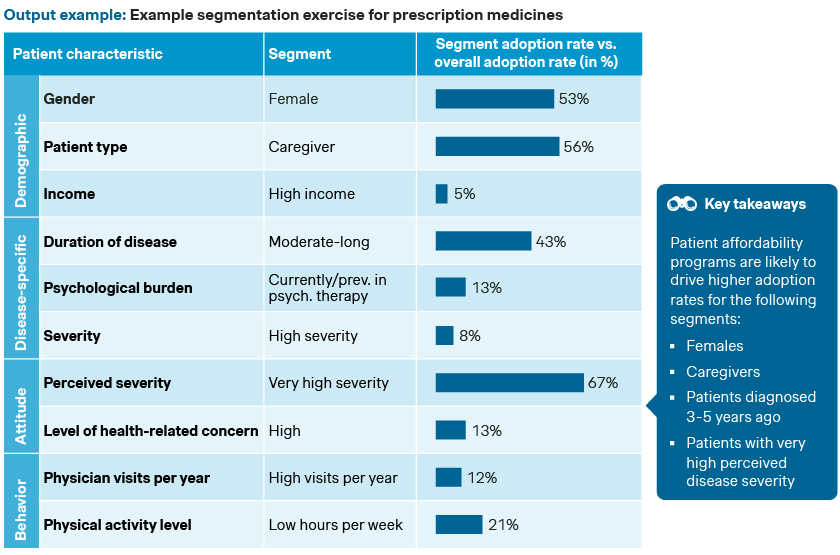
Which patients need financial support to access medications and for whom could support programs change behavior?
To design and implement an effective patient affordability program, it is important to get a deeper understanding of the population that is most likely to utilize and benefit from it. While patients without insurance coverage and/or lower socioeconomic status are often considered target groups for such programs, the target patient group should not only be determined by reimbursement status and income alone.
Identifying and understanding the target patient population should also include a detailed segmentation exercise. This should focus on assessing underlying drivers and barriers in patient adoption and defining segments based on demographics, health risk, behavior, and attitude.
Segmentation will help inform which types of patients are most likely to use provided programs. It also allows manufacturers to make strategic decisions when designing affordability programs and selecting implementation partners to ensure the relevant populations are reached.
Evaluate optimal program durations
What is the role of the affordability program in the product’s lifecycle?
Both short and long-term affordability solutions can be helpful in addressing patient concerns, driving health equity, and increasing therapy access. Short-term affordability programs are most often used to help bridge funding gaps prior to reimbursement decisions. Long-term programs are typically explored once reimbursement decisions have been made and funding gaps remain.
Short-term affordability programs can pose a risk to payer negotiations in some markets, as prices provided in these “stop-gap solutions” may be leveraged by payers. Discounts provided within the solution may become an underlying stipulation for reimbursement.
This risk does vary by market – while early access programs have not been observed to have posed this risk e.g., in France on a broader basis, this remains a concern in markets such as e.g., South Korea and Hungary where prices provided in patient affordability programs can be considered in negotiation proceedings.
There are also important reputational risks to consider for both program types. If support is withdrawn from a population that remains in-need after reimbursement, the reputational consequences may have a downstream effect on patient and/or provider product perception or the company as a whole.
Regardless of their role within the product’s lifecycle, affordability programs should be continuously evaluated for their efficiency and commercial impact. Without continuous oversight, programs may become non-viable to manufacturers, impacting overall patient access.
Identify the right price for patients
What is the willingness to pay for the product and the anticipated price elasticity within the target population? Is this supported by ability to pay?
Setting the “right price” within an affordability program should consider financial viability as well as impact on ability to achieve goals of broader patient access and health equity (factoring in patients’ willingness and ability to pay). The same level of support does not always result in proportional uptake between markets or patient populations.
Patient price sensitivity can be impacted by several different factors, including historical healthcare spend, income levels, and perceived product need, as well as cultural trends. Starting with a deeper understanding of what is driving the price elasticity curve is key to developing patient affordability programs that will actually support patient access. It will also help identify quick wins (where relatively small cost savings to patients will improve patient access) and challenging endeavors (where financially unviable programs will be needed to create a meaningful impact on access, suggesting need for charitable program partnerships).
Identify the right program
Which type(s) of affordability program(s) are feasible given patient, market, and product dynamics?
There are many different types of patient affordability programs that manufacturers can choose from. Your choice of program should be based on:
- Product characteristics (e.g., chronic, acute, preventative, niche target population, etc.)
- Legal or payer stipulations (e.g., direct promotion of such programs is prohibited, or payment support cannot be provided for reimbursed products)
- Market dynamics (e.g., precedence and/or patient appetite for such programs)
- Implementation feasibility (e.g., availability of third parties for implementation support, ability to provide target discounting levels within the program)
- Patient (and physician) attractiveness
| Patient affordability programs | Real-world examples | |
|---|---|---|
| Discounted goods |
|
|
| Copay Assistance |
|
|
| Non-discount payment solutions |
|
|
| Free goods |
|
|
Build the right ecosystem
What gaps in the current ecosystem may influence adoption behavior?
Depending on other challenges in the patient journey and established infrastructure available, additional services may be required to maximize the impact of affordability programs on patient access. Added services should aim to address remaining barriers to uptake and/or program implementation, including patient perceived unmet need, hurdles in physical access to products, program automation and delivery to patients, complexities associated with health insurance, etc. As always, manufacturers should conduct an assessment to ensure the viability of added services and alignment with their strategic goals.
Case example: Ecosystem building in Mexico
Program: MAZSalud
Manufacturer: AstraZeneca
Market: Mexico
Indication: Undefined
In addition to providing financial support patients through free goods, AstraZeneca has built a supportive ecosystem within the program to ensure other access barriers, aside from medication costs, do not impact patients. Additional elements of the program include:
- Information, education, and disease awareness tools to ensure patients are updated and improve adherence to treatment - Free remote nutritional consultation
- Home delivery of medications at no additional cost
- Assistance with insurance claim processing
- Free lab tests
- Discounts on tests and laboratory studies
- Free remote psychological and emotional coaching
- Guidance on at-home administration of medication
Choose the right partner to deliver your solutions
Are there any opportunities or requirements for outsourcing implementation of patient-facing programs?
As part of building the right ecosystem for patient affordability solutions, developing external partnerships may be beneficial, if not necessary. In some markets, such as Thailand, legal restrictions placed on manufacturers create implementation hurdles to offering direct patient support programs that can only be overcome with third-party partner support.
In these markets, there are often established vendors that implement patient-facing programs on behalf of manufacturers. However, vendor costs are often a key concern, along with reputational risks associated with relying on a third-party vendor. Manufacturers should always conduct detailed vetting of any potential partners to help reduce these risks.
In some markets, partnerships can help to increase program efficiency or reduce implementation costs, making them attractive options for manufacturers, even if not legally required. For example, in Mexico, pharmacies often implement their own loyalty card program to help alleviate costs for patients. In this case, manufacturers can simply opt into the program and utilize the established infrastructure set up by the pharmacies. It is important to understand where potential partners have had past success to better identify and plan for future engagements.
Finally, partnerships are not meant to just address implementation challenges. They can also be used to help cover costs, distribute the product, increase patient engagement, and raise awareness of support programs in place. Partnerships with government agencies, NGOs, payers, and physicians can all be beneficial and should be explored if necessary.
Act now – Unlock better growth with a sustainable patient affordability strategy
Concern regarding healthcare affordability is rising globally. Manufacturers must be ready to react and adapt to changing patient needs, offering the right programs to the right patient groups, at the right time and under the right product and market conditions.
Proactive development of effective and sustainable affordability strategies in key global markets will continue to be integral to product success and help improve health equality in the future.
Let’s work together to plan an affordability strategy for your brand. One that not only unlocks better growth for your company, but also better health outcomes for patients and society as a whole. Reach out to Simon-Kucher today.
Better Market Access
The role of better market access is to remove any hurdle that prevents or hinders patients from receiving available treatments. In the right place, and at the right time.
Today, the impact of market access spans clinical development, regional commercial activities, patient engagement, and post-launch compliance. Yet, for many pharmaceutical companies, planning for commercialization only truly begins when a drug has been submitted for approval — far too late in the process.
Get to know our insights on local trends, regional and global developments and global to local excellence.